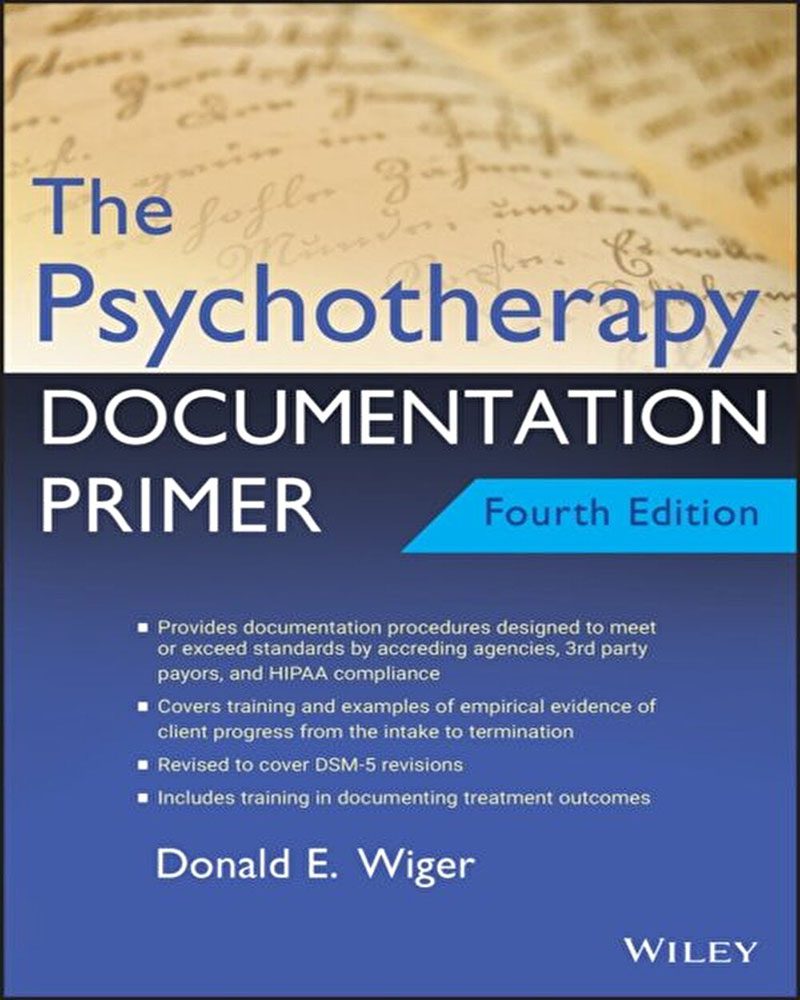
Everything you need to know to record client intake, treatment, and progress―incorporating the latest managed care, accrediting agency, and government regulations
Paperwork and record keeping are day-to-day realities in your mental health practice. Records must be kept for managed care reimbursement; for accreditation agencies; for protection in the event of lawsuits; to meet federal HIPAA regulations; and to help streamline patient care in larger group practices, inpatient facilities, and hospitals.
The standard professionals and students have turned to for quick and easy, yet comprehensive, guidance to writing a wide range of mental health documents, the Fourth Edition of The Psychotherapy Documentation Primer continues to reflect HIPAA and accreditation agency requirements as well as offer an abundance of examples.
Fully updated to include diagnostic criteria of the DSM-5, The Psychotherapy Documentation Primer, 4th Edition is designed to teach documental skills for the course of psychotherapy from the initial interview to the discharge. The documentation principles discussed in the text satisfy the often-rigid requirements of third-party insurance companies, regulating agencies, mental health licensing boards, and federal HIPAA regulations. More importantly, it provides students and professionals with the empirical and succinct documentation techniques and skills that will allow them to provide clear evidence of the effects of mental health treatment while also reducing the amount of their time spent on paperwork.

Reviews
There are no reviews yet.